Imagine keeping a file folder of up-to-date information about every physician working across a healthcare organization — dozens and dozens, if not hundreds of them. Now, imagine that their information needs to be checked and updated periodically throughout the year… but no one is on the same schedule. Moreover, you’re constantly adding new files for new people. If this sounds like a headache, that’s because it is. Thankfully, it’s a headache that credentialing software is specifically designed to remedy.
If your healthcare organization is still credentialing through pen and paper — and roughly two-thirds of organizations are — it’s time to embrace the power of technology. Let’s explore what healthcare credentialing software can do for you.
Uncover the secrets to speeding up your credentialing process here.
What Is Healthcare Credentialing Software?
Healthcare credentialing software automates and streamlines the process of verifying and validating the qualifications and credentials of healthcare professionals. It’s commonly used by credentialing specialists at hospitals, urgent care centers, and other healthcare facilities to ensure providers meet the necessary requirements and standards for employment and practice.
Healthcare credentialing involves verifying various aspects of a healthcare professional’s background, including their education, training, certifications, licenses, work history, malpractice history, and any other relevant credentials. Because these facts require primary source verification, credentialing is often a complex, time-consuming process. Credentialing software helps simplify and expedite it!
How Is Credentialing Software Used?
Healthcare credentialing software provides a centralized platform where organizations can collect, store, and manage all the necessary data and documentation related to credentialing. Credentialing software usually includes features such as:
Application Management
The software allows healthcare providers to submit their credentials and applications online, eliminating the need for paper-based processes and expediting the timeframe for verification.
Verification and Background Checks
Software automates the verification process by directly accessing databases and primary sources to confirm the accuracy and validity of credentials, including licenses and certifications.
Document Management
Cloud-based software enables the storage, organization, and retrieval of documents related to healthcare providers’ credentials. This can include résumés, licenses, diplomas, and insurance (payer) enrollments.
Compliance Tracking
Credentialing software helps organizations stay compliant with regulatory requirements by tracking and managing the expiration dates of licenses, certifications, and other credentials.
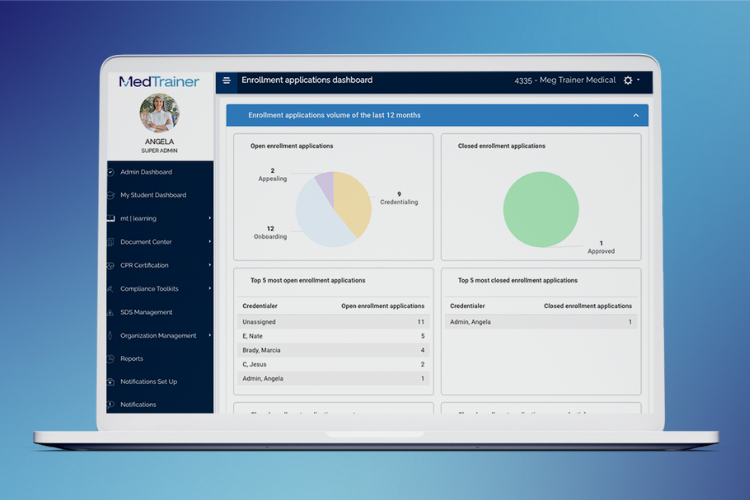
Reporting and Analytics
Software can quickly generate reports and analytics to provide insights into the credentialing process, including timeframes, completion rates, and potential bottlenecks.
Communication and Collaboration
Credentialing software can facilitate communication between credentialing staff, healthcare providers, and other stakeholders involved in the process, to ensure efficient collaboration and information exchange.
Generally speaking, credentialing software makes a credentialing specialist’s job easier by bringing everything together and creating a single source of truth for compliance standards.
What Are the Benefits of Credentialing Software?
As mentioned, credentialing can be a somewhat tedious process, since primary source verification often means being at the mercy of others to confirm physician information. While credentialing software can’t necessarily expedite the verification process, it does provide many back-end benefits that benefit both credentialing specialists and the organization, from a compliance standpoint:
Time-Saving
Credentialing software automates many manual tasks involved in the credentialing process, such as data entry, document management and verification. This saves time and allows organizations to complete the credentialing process faster. On average, using credentialing software like MedTrainer can help complete credentialing three weeks faster!
Revenue Opportunities
Efficient and organized credentialing enables healthcare organizations to seize more revenue opportunities. By ensuring that providers are properly credentialed, organizations can participate in more insurance networks, expand their patient base and attract new revenue streams.
Increased Staff Retention
The streamlined credentialing process facilitated by software reduces the administrative burden on employees. This leads to happier and less-stressed staff members, which, in turn, increases staff retention rates. Improved job satisfaction contributes to a more positive work environment.
Improved Continuity
When staff members leave or new hires join an organization, credentialing software helps maintain continuity. The software securely stores all credentialing information, making it easier to transition responsibilities and ensure that new staff members are appropriately verified.
Flexibility
Many credentialing software solutions like MedTrainer are cloud-based, allowing users to access and manage credentials from anywhere with an internet connection. This flexibility enables remote work capabilities and ensures that credentialing processes can continue seamlessly even in the event of disruption.
Shorter Training Period
Credentialing software is designed to be user-friendly and often includes intuitive workflows that guide users through the credentialing process step-by-step. This ease of use reduces the training period required for new employees, allowing them to become productive and proficient in credentialing tasks more quickly.
How to Select Healthcare Credentialing Software
As healthcare becomes an increasingly digital frontier, options for healthcare credentialing software have expanded. When it comes to choosing a credentialing software solution that supports your organization’s credentialing needs, consider the following criteria:
- Cloud-based system. Today’s digital healthcare lives in the cloud. When it comes to credentialing, organizations need access anywhere — no more printing out papers and risking losing paper files that providers share. With everything in a centralized repository, compliance also becomes easier.
- Provider profile management. Especially for managing multiple providers across multiple locations, profile management is crucial. Look for software that compiles and organizes documents and information in one location, for ultimate visibility and continuity when the time comes to credential or recredential.
- Automation of manual tasks. Credentialing is ongoing. Look for software that automates things like email reminders to providers, recredentialing reminders, and monthly exclusion checks. Choose software that empowers you to be proactive instead of reactive, and keeps you ahead of deadlines.
- Real-time reporting. Compliance reporting is a crucial aspect of credentialing software. Evaluate software on the basis of its ability to provide you with relevant, timely reporting across a variety of metrics. With real-time reporting, it becomes easier to assess the credentialing landscape at any given moment.
- Configurable workflows. Credentialing isn’t always a linear process, and you might find yourself waiting on verifications or approvals out of order. Choose software that allows you to configure workflows that make sense for your process, to ensure consistency across every provider’s credentialing process.
With these factors in mind, look into different credentialing software providers and identify the ones with features and benefits that you ranked highly. From there, it’s simply a matter of choosing the system that’s best for your needs!
If you’re looking for medical credentialing software, find out why MedTrainer should be on your list!
Complete credentialing 3 weeks faster
