Using a provider credentialing service removes the stress and frustration associated with the process and often results in faster credentialing and enrollment. But, credentialing services pricing is a key factor in whether it fits your healthcare organization correctly.
Because of its complexity, credentialing costs can vary significantly depending on the services offered and the pricing model the credentialing services vendor uses. Keep reading for a complete breakdown of pricing for credentialing services and ensure your healthcare organization gets the value you expect.
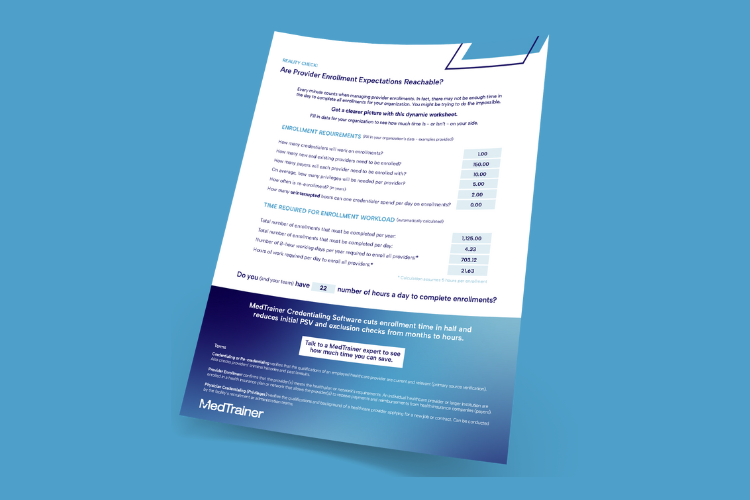
Fill in this worksheet to determine how many hours your enrollments should take.
What To Look for in Credentialing Services
When evaluating credentialing services, it’s crucial to understand that not all vendors offer the same level of service. “Completing enrollments” can mean different things depending on the service provider. For some, this might mean merely submitting applications, while others include comprehensive payer follow-up and navigation through the enrollment decision process, such as approvals, rejections, and denials. Ask questions, thoroughly review the contract, and confidently decide.
Here’s a quick list of what to look for when selecting a credentialing services vendor:
- State-specific expertise and experience
- Network relationships
- Visibility into the process through an online platform
- Adherence to NCQA standards
- Turnaround time that works for your organization
- Flexibility and scalability
- Accessible customer support and a dedicated point of contact
- Comprehensive monthly reporting
Understanding Credentialing Services Pricing
There’s a wide range of medical credentialing services pricing, and it is usually one of two models: a la carte or all-inclusive. Understanding these models and their features can help you make the best decision for your organization.
A la Carte Pricing
With a la carte pricing, you pay for each service individually. This can feel like usage-based pricing since you’re only paying for what you think you need. However, without clear definitions, you may find yourself paying extra for essential steps like payer follow-up or correcting application errors—services that most organizations actually need but aren’t always included upfront.
For example, if a credentialing service vendor does not clarify what is included, you may pay extra for critical steps like follow-ups or resolving application errors. Then you’re in a situation where you’re arguing over what should have been done and a provider’s enrollment is even more delayed than if you had done it yourself.
Here are some services that might be charged individually:
- Application submission
- Primary source verification
- Payer follow-up
- Background checks
- License verification
- Privileging
All-Inclusive Pricing
On the other hand, all-inclusive pricing covers a comprehensive range of services for a single fee. Even if there are parts of the coverage you think you might not need, this model is often more cost-effective in the long run.
The greatest value comes from the seamless, end-to-end management of the credentialing process, which helps avoid costly delays and administrative burdens. Plus, this option is perfect for organizations that are growing or where staffing changes could cause major slowdowns.
All-inclusive pricing typically indicates a more comprehensive service, ensuring that every aspect of the credentialing process is handled professionally and efficiently. Even if it seems like you’re paying for services you don’t need, all-inclusive pricing often prevents surprise add-ons. By covering every step of the credentialing process, you gain cost predictability and assurance that critical tasks won’t fall through the cracks or lead to unexpected invoices. This transparency and reliability are invaluable for healthcare organizations focusing on the patient experience rather than administrative hassles.
Calculate the Value of Credentialing Services
Ultimately, the question isn’t whether you’re paying for things you don’t need. It’s whether the pricing model ensures all the essentials are covered without nickel-and-dime charges, and whether the speed and accuracy of the service outweigh the cost.
Instead of focusing on credentialing services pricing, let’s think about the value. Delays in the credentialing process can be extremely costly. According to industry statistics, each day a provider cannot see patients due to credentialing delays, which can cost a healthcare organization approximately $9,000.
Let’s say you’re paying $5,000 per year for credentialing services for all of your providers. Even if you’re paying $10,000 per year – if one provider is credentialed just one day faster, you’ve more than paid for your investment. Imagine if 10 new providers are credentialed 2 days faster each. They’re able to make an additional $180,000 for your organization. That’s worth the $5,000-10,000 you paid for the services, right? And you didn’t have the headache.
MedTrainer Credentialing Services customers save, on average, three weeks per provider.
See how we do it in this 2-minute video.
Choose MedTrainer Managed Credentialing Services
MedTrainer Credentialing Service relies on our robust credentialing platform to provide complete visibility of the credentialing process. With MedTrainer’s Managed Credentialing Services, you benefit from:
- Comprehensive Service: MedTrainer’s platform manages every step of the application submission process, from payer follow-up to recredentialing.
- Transparency: Real-time updates and visibility into every part of the process ensure you are always informed.
- Efficiency: MedTrainer streamlines the credentialing process, reducing delays and administrative burdens and allowing you to focus on patient care.
Schedule a demo today or talk to a MedTrainer Credentialing Services expert.
 Learning
Learning