Staying up to date on provider credentials can be time-consuming and complicated. Fortunately, credentialing management software can help healthcare practices streamline the process of managing and verifying credentials for both individual practitioners and organizations. Credentialing management software helps keep practices compliant and organized, while reducing the amount of work involved for administrators and staff.
Here’s what to look for in your credentialing management software.
What Is Credentialing Management Software?
Credentialing management software is a specialized digital tool designed to centralize the process of managing and verifying credentials for individuals or organizations. It serves as a comprehensive platform to store, update, and monitor credentials such as licenses, certifications, degrees, and other qualifications. The software is commonly used in various industries, including healthcare, education, and professional services, where maintaining up-to-date and accurate credentials is crucial for compliance and quality assurance.
By automating the credentialing process, this software reduces manual errors, enhances efficiency, and ensures regulatory compliance. It typically includes features such as document storage, credential expiration alerts, verification tools, and reporting functionalities. Overall, it’s an indispensable tool for simplifying complex credentialing tasks and maintaining a well-organized and qualified workforce or network of professionals.
Complete credentialing 3 weeks faster
How Does Credentialing Management Software Streamline the Credentialing Process?
Credentialing management software streamlines the credentialing process through various efficient features that enhance speed, accuracy, and organization. Here are some of the key features:
Information at Your Fingertips
One of the key advantages of credentialing management software is the availability of information. With an online dashboard, users can access essential data and progress updates instantly. This real-time accessibility allows administrators, providers, and stakeholders to receive immediate answers to inquiries, track the progress of credentialing tasks, and prioritize activities based on expiration dates of provider credentials or certifications. This not only facilitates quicker decision-making; it also improves the overall responsiveness of the credentialing process.
Centralized Document Management
Centralized document management is another critical tool. Having a single location for all provider data, documents, and communication simplifies the credentialing process by eliminating the need to search through various physical or digital repositories. This centralized approach ensures that all relevant information is readily available and easily accessible. The software typically accommodates over 500 data points of provider information required for credentialing.
Administrators can customize the list of required documents for each location or facility, ensuring consistent compliance standards across the organization. This not only helps maintain uniformity but also simplifies the process for affiliated providers, as they use the same preset document list for submission. Moreover, the platform often allows providers to electronically upload documents directly, reducing delays caused by traditional paper-based methods.
Reduced Processing Time
Using predefined workflows expedites the credentialing process. These workflows consist of predefined sequences for tasks, ensuring that one task automatically starts as soon as the preceding task is completed. This automation significantly reduces manual intervention, prevents bottlenecks, and keeps the process moving forward seamlessly. Additionally, automated reminders and notifications prompt both administrators and providers to stay on track with their responsibilities, further reducing the time it takes to complete the credentialing process.
What Are the Key Functionalities of Credentialing Management Software?
Credentialing management software offers a range of functionalities that simplify the process of managing and verifying credentials for healthcare professionals.
Verification of Credentials and Licenses for Healthcare Professionals
One of the primary features is the automated verification of credentials and licenses. Instead of manually searching through various websites and pages, the software streamlines the verification process by automatically cross-referencing data to ensure that healthcare providers have valid DEA and state licenses. This feature saves valuable time and effort, reducing the burden of administrative tasks and ensuring accurate and up-to-date information.
Highly Customizable Reports
Advanced software also provides highly-customizable reports, offering valuable insights to support informed decision-making:
- Credentialing report. This keeps administrators up to date with their providers’ clinical privileges, verifications, exclusions, and documents. It provides a comprehensive overview of each provider’s credentials and status within the organization.
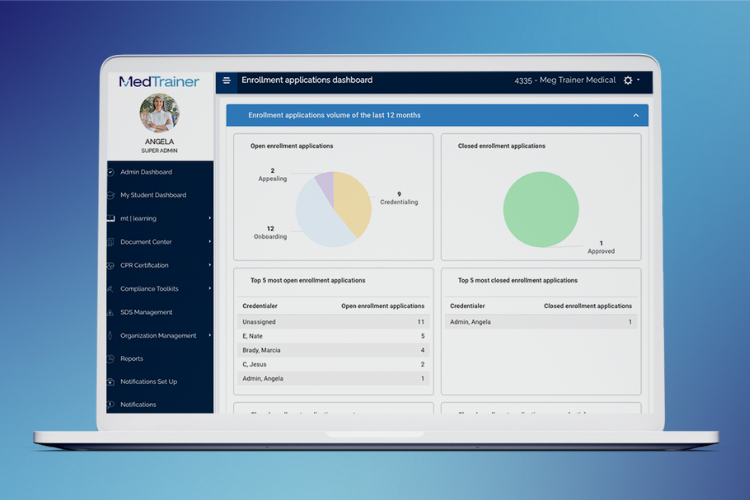
- Enrollment applications dashboard. The Enrollment Applications Dashboard is another critical report, presenting a comprehensive view of the enrollment process, including performance metrics, highlights, and potential risks. This allows administrators to promptly address any issues.
- Exclusion reports. Exclusion reports allow administrators to quickly check the eligibility of providers to work, ensuring they are not listed in the System for Award Management (SAM) or the Office of Inspector General’s List of Excluded Individuals/Entities (OIG-LEIE). This helps maintain compliance and safeguards the facility from potential legal issues.
- Licenses report. A licenses report facilitates the tracking of all licenses and certifications that require continuing education or refreshers. This ensures that providers are always up to date with their qualifications, and it helps organizations avoid any lapses in compliance.
View our guide, Compliance Reports You Can’t Live Without, for step-by-step instructions on creating all the reports listed above, and more.
Track Expirations and Renewal Dates
The software automatically tracks the expiration dates of healthcare professionals’ credentials, such as licenses and certifications. By providing real-time notifications up to 120 days before expiration, administrators eliminate the risk of overlooked expirations, ensure timely renewal, and reduce the administrative burden on credentialing staff.
Streamline Provider Enrollment
This feature streamlines the provider enrollment process by centralizing and automating tasks. It offers a unified platform for providers to submit applications and documents electronically, minimizing paperwork. Automated follow-up features send reminders and notifications to both administrators and providers, expediting the enrollment process. The software’s interactive dashboards allow real-time monitoring of enrollment status, enhancing revenue cycle management and freeing up resources for more critical tasks.
MedTrainer Credentialing Software Simplifies the Process
MedTrainer Credentialing organizes and accelerates your process with cloud software and a team of specialists who can manage the process for you. Customers say MedTrainer speeds up credentialing by three weeks on average — per provider. All the data you need to make business decisions is in one place. From provider data and files to upcoming action dates and automatic reminders, MedTrainer provides a single place to enter, import, and store mandatory provider information and documents based on NCQA guidelines.
Want to learn more about how credentialing software can simplify the process in a major way? Schedule a free demo of MedTrainer today!
