Credentialing can make or break a healthcare organization’s revenue. To keep the money flowing, more organizations are implementing software to speed up the tedious process. Of course, one of the first questions is: What does credentialing software cost?
Herein lies the paradox: Healthcare organizations believe they can’t afford digital credentialing software, but more than a third of MedTrainer poll respondents say credentialing delays cost them money. In addition, 26% believe credentialing delays increase the risk of compliance violations that may cost more in the long run.
So, when evaluating healthcare credentialing software costs, it’s important to weigh it against money saved and the return on investment the organization will receive when providers are reimbursed. Here’s a look at how to do that.
What is Credentialing Software?
Credentialing verifies that an individual, institution, or organization meets established standards and is recognized to carry out a designated role or function. Credentialing management software improves credentialing data management, automates workflows, and speeds up the process.
Credentialing software offers many benefits. It helps organizations complete credentialing and enrollment faster, reduce waiting time, and increase accuracy. It is used by healthcare organizations to simplify primary source verification, payer enrollment, privileging, ongoing recredentialing processes, and more. Standard features of provider credentialing software include provider profile management, automated notifications and reminders, customizable reporting and dashboards, automated exclusions monitoring, and customizable workflows.
What Does Credentialing Software Cost?
Most software subscriptions charge by month for a specific number of users or a level of access. You can expect to pay between $20 and $50 per month per user. Both your credentialing staff and the providers they are credentialing would be considered users. So, if you have 15 people who need access to the data, you would be paying between $300 and $750 per month. That’s an annual cost of $3,600 to $9,000.
Is Credentialing Software Worth It?
According to a study by Merritt Hawkins, one physician’s revenue for your organization is an average of ~$2.3M a year, or about $9,000 a day. Your organization is losing potential revenue for every day a provider is unable to practice because he is not credentialed or enrolled.
Even if you choose credentialing software that costs $9,000 per year, if you can enroll one provider one day faster, you’ve already covered the cost of the entire year.
But can credentialing software really speed up your process and save you money? Let’s examine a few scenarios.
Manual vs. Automated
Automated credentialing is the key to getting time back so your organization can start earning sooner. Take exclusion checks, for example. Checking every database every month is a pain. Automated exclusions monitoring in credentialing software takes care of this tedious task, sending an email when a provider’s status changes. This takes an hours-long process down to seconds. You can experience similar time savings with automated license verifications and reminders to submit documents.
When every day costs an organization $9,000, saving just a day or two here and there makes credentialing software a great investment.
Reduce Time Spent Waiting
It probably seems like you’re always waiting—waiting for providers to share documents or payers to respond. If you get a provider’s documents or a payer response three days faster than your current process, the provider can bring in $27,000 more in revenue.
Can credentialing software help you get quicker responses?
Credentialing software offers electronic document requests, so the provider gets a link to upload the required documents securely to a portal. Reminders are sent until all required documents are uploaded. It’s easier for providers to upload documents electronically instead of printing, delivering, or mailing. Plus, a professional-looking request can prompt quicker action. Regarding payers, most credentialing software users include payer follow-up in their workflow with automated reminders. Remember the old saying, “The squeaky wheel gets the grease?”
Increasing Accuracy
The credentialer forgot to include the LOI in the enrollment packet. You’re already waiting for the payer to review the submission—let’s say it’s been two weeks. That missing LOI may force you to resubmit the application and start over. It takes 10 days to fix the mistake. You’ve lost $90,000 in potential revenue.
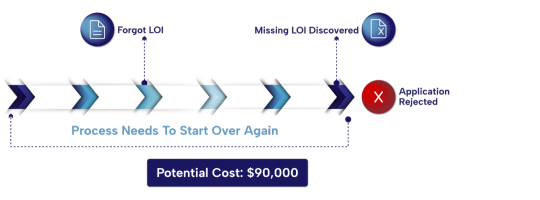
Using credentialing software, you have a standard list of documents you electronically request from providers, and the LOI is one of the documents. Since the provider gets automatic reminders until all requested documents are uploaded, you can be confident you’ll get the LOI before you get too far into the packet. Plus, using the interactive checklist in credentialing software ensures you don’t forget anything — including the LOI.
Get the tools you need to eliminate delays in your provider enrollment process.
Choosing the Best Healthcare Credentialing Software Solution
There’s no “best” method of credentialing providers, although it’s not advisable to try managing the process using paper and spreadsheets. As you’ve seen, credentialing software costs do not outweigh the benefits software provides — you just need to choose the best software for your healthcare organization.
MedTrainer customers say they save 15 working days credentialing one provider. At $9,000 a day, that’s $135,000 each provider can earn when the organization uses MedTrainer Credentialing Software. All provider data is in one location, and providers can upload their documents. Automation and checklists keep the credentialing process on track so you can eliminate costly delays.
If you want to understand how credentialing delays affect your provider enrollment process, try our Credentialing Reality Checklist for a comprehensive look at your timeline for enrolling providers. If this sounds exactly what you need, MedTrainer can help. Contact us today.
