Ten hours. That’s how long it takes most organizations to credential a single provider, according to a 2023 MedTrainer poll. Now multiply that by the number of providers in the organization, then by the number of payers with whom you’re verifying credentials.
The sheer volume of verifications and time needed to complete them almost demands a robust digital credentialing system. Yet only a third of organizations surveyed in the MedTrainer poll use a digital credentialing solution, with cost being the top inhibitor for 35%. Reticence to let go of manual processes – It’s how we’ve always done it – is a close second at 29%.
Herein lies the paradox: Healthcare organizations believe they can’t afford a digital credentialing solution, but more than a third of poll respondents say credentialing delays cost them money. In addition, 26% believe credentialing delays increase risk of compliance violations that may cost more in the long run.
Conquer the Credentialing Paradox
Credentialing isn’t going to get easier. There are dozens – if not hundreds – of reasons the credentialing process can be delayed. The continued growth of disparate online portals, additional payer and government restrictions, a continuing increase in telehealth, reluctance of employers to make credentialing a standalone position, and on and on.
This is where healthcare credentialing software pays dividends. The 33% of companies surveyed who are using a digital credentialing solution are miles ahead of those stuck on manual paper and computer entry. Digital credentialing solutions help maintain accurate provider information (and reduce human error), reduce workloads on already-stretched staff, and mitigate risk. According to 60% of respondents, sending emails and collecting documents is the hardest part of their job. Many digital solutions can automate this tedious process.
Here is how digital credentialing software helps clear hurdles by creating efficiencies and clarity:
- Time savings. Adding automations to the credentialing process significantly reduces the time required to gather, verify, and update provider information. This enables organizations to expedite onboarding and maintain compliance with less administrative burden.
- Compliance and regulatory adherence. Automated exclusions monitoring removes the tedious manual task of checking federal and state exclusions databases. This protects patients and reduces the risk of non-compliance and associated penalties.
- Real-time updates. Reminders are particularly important for staying on top of expiring licenses, certifications, and other time-sensitive credentials.
- Centralized documentation. Storing provider credentialing documentation — such as licenses, certifications, and training records — in a centralized digital repository ensures easy access and simplifies the auditing process.
- Enhanced security. Digital credentialing platforms offer security features that protect sensitive provider information from unauthorized access.
- Provider profiles. Comprehensive profiles capture all relevant information, and track empty fields and missing documents to speed up the process.
- Streamlined communication. Communication tools can enable direct communication between providers and the credentialing team, streamlining the verification process.
- Stronger provider relationships. Providers who have a streamlined, faster credentialing process are more likely to stay with the organization.
Complete credentialing 3 weeks faster
Accelerate Your Provider Credentialing with MedTrainer
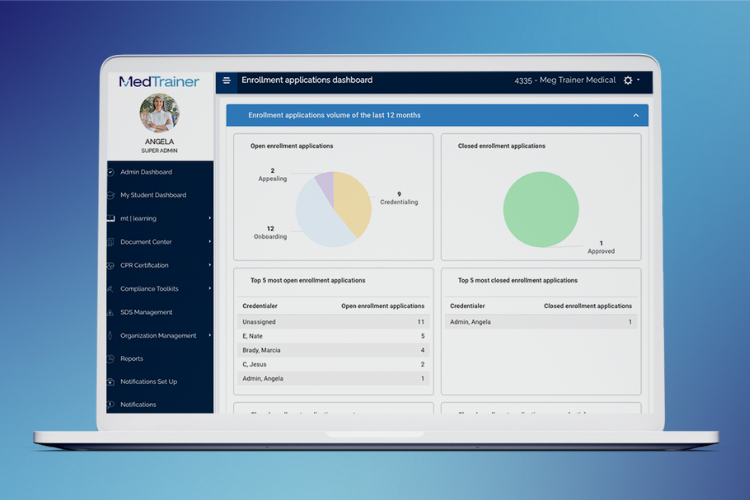
Quality provider credentialing software can dramatically improve your organization’s processes. MedTrainer organizes and accelerates your process with cloud software and a team of specialists who can manage the process for you. Customers say that on average, MedTrainer speeds up credentialing by three weeks — per provider! This means faster speed-to-care and less risk on the part of the organizations employing them.
With MedTrainer Credentialing, all the data you need to make business decisions is in one place. From provider data and files to upcoming action dates and automatic reminders, MedTrainer provides a single place to enter, import and store mandatory provider information and documents based on NCQA guidelines. Explore MedTrainer’s credentialing features today!
