The Administration for Community Living (ACL) recently updated the Older Americans Act (OAA) for the first time in 34 years to ensure older adults receive broader services and support from state and territorial agencies – and the healthcare organizations that provide services through them. The final OAA rule took effect March 15, 2024, and regulated agencies have until Oct. 1, 2024, to comply with the updates.
State and area agencies on aging (AAAs) must also ensure healthcare organizations – including but not limited to Native American health agencies, home health, and long-term care facilities – comply with several provisions of the OAA final rule that include “service providers.” If your healthcare organization works with OAA-regulated agencies, it may be time to refresh employee compliance training around emergency preparedness, preventing elder abuse, and avoiding conflicts of interest.
What Is the Older Americans Act?
First passed in 1965, the OAA authorizes a wide range of programs and services focusing on helping older adults age in place. These services include home-delivered and congregate meals, support for family caregivers, preventive health services, personal and home care services, transportation, legal assistance, elder abuse prevention, and more. In addition, the OAA provides ombudsman services for people who live in long-term care facilities. There are nearly 123M Americans age 60 and older, many of whom need ongoing in-home or assisted-living care and may qualify for OAA program assistance.
Important Updates for OAA Service Providers
State agencies set policies and procedures that service providers and AAAs must follow, including what services may be provided and the limitations on the frequency, amount, or type of services. States are still ratifying the OAA language and creating policies to manage service delivery within their borders.
Here are three provisional changes that align regulations to the current statute, address issues that have emerged since the last update, and clarify several requirements:
- Conflict of Interest: Prohibits the officers, employees, or agents of the OAA program from soliciting or accepting gratuities, favors, or anything of monetary value from contractors – healthcare organizations as service providers – except where policies and procedures allow for situations where the financial interest is not substantial, or the gift is an unsolicited item of nominal value.
- Emergency Preparedness: State agencies and AAAs must establish emergency plans and have policies and procedures for communicating and coordinating with state, tribal, and local emergency management. Healthcare organizations acting as service providers must be prepared to follow state and AAA plans.
- Preventing Elder Abuse: Provides funding to state agencies to train healthcare providers, law enforcement officers, and other professionals to recognize and respond to elder abuse.
How To Keep up With a Moving Target
Implementing policy changes that originated from federal and state agencies may feel like a moving target throughout the implementation phase of the Final Rule. Here are suggestions for ensuring a clean “paper trail” to manage the lifecycle of policies, job aides, and other guidance resources:
- Utilize electronic policy and document management systems to ensure managers and frontline staff have the most up-to-date versions of all related documents.
- Record and manage document versions and collaborate with key stakeholders to ensure organization-wide adoption.
- Track and monitor employee acknowledgments and provide staff with immediate access to important documents and instructions.
Emphasize Elder Abuse Prevention Training
One in 10 people 60 years and older experience some form of elder abuse every year in the U.S. The majority of abuse is done by caregivers either in the elder’s home or a care center. The OAA final rule designates more funding to prevent elder abuse, emphasizing training clinical staff and caregivers to identify and report violations.
All 50 states and the District of Columbia have Mandated Reporter laws that govern elder abuse reporting. Laws and abuse definitions vary by state. In Florida, elder abuse can be a first-degree felony, resulting in up to 30 years in prison. Arizona requires any person with “responsibility for the care of a vulnerable adult and who has a reasonable basis to believe that abuse, neglect, or exploitation of the adult has occurred….”
Training is vital to help healthcare professionals and caregivers identify, report, and prevent elder abuse. Many states offer training as part of ongoing education to help clinical, non-clinical, and family members recognize and report adult maltreatment. Check state requirements to see what roles are considered Mandated Reporters and if training is available.
Deliver Facility and Caregiver Training With MedTrainer
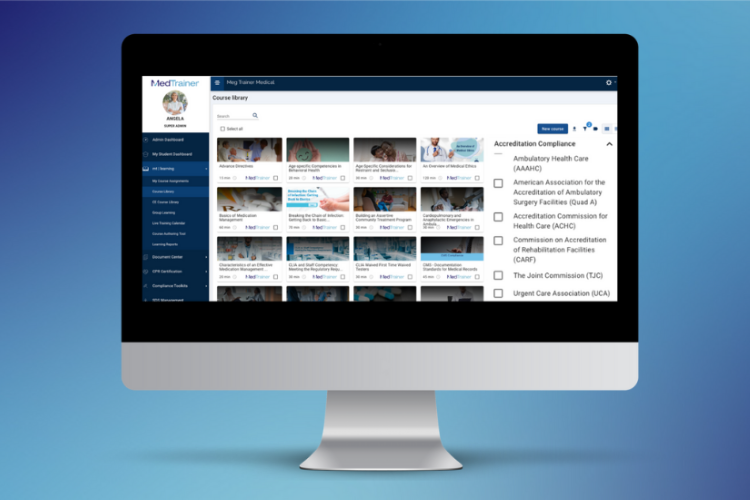
Healthcare organizations looking to use OAA grants to extend care to at-risk and vulnerable populations can leverage MedTrainer Learning to offer state-specific training and coursework unique to clinical and non-clinical roles by location and facility type. Organizations can create facility- or role-specific content using MedTrainer’s Course Authoring Tool.
Our all-in-one platform is built for healthcare, and thousands of organizations use MedTrainer to simplify training and compliance needs. Courses that are designed to meet multiple standards, and you can create or upload facility-specific courses to align with OAA guidelines.
Simplify compliance training with MedTrainer Learning
MedTrainer offers an all-in-one compliance solution combining learning, documentation, and credentialing. Experts will help your organization ensure that training is complete and compliant. Learn more about MedTrainer.