From medicines to equipment, there’s a long list of costs that make the healthcare industry expensive to manage. One expense that some individuals are incredibly familiar with — and maybe wish they weren’t — is the cost to credential a physician.
Provider credentialing is crucial for the success of healthcare organizations, but it can push an already strained budget to the brink. Credentialing can put money in your pocket, but the old adage also strikes true: it takes money to make money. So how much does credentialing truly cost?
Preserve your revenue by speeding up your enrollment process. Watch the on-demand webinar.
What Is Medical Credentialing?
Medical credentialing is the rigorous procedure of verifying that a physician possesses the necessary qualifications and experience to perform their job competently and safely. This process involves many steps, including:
- Primary source verification ensures that a physician’s educational and training credentials are authentic and up-to-date.
- Exclusion checks ensure the physician is not on government or industry exclusion lists for prior malpractice.
- Payer enrollments are necessary to ensure a physician is approved to provide services to patients covered by various health plans.
- Privileging is when a physician has permission to perform specific medical procedures or services.
- Recredentialing is the periodic renewal of credentials to ensure ongoing compliance with regulatory and quality standards.
By completing these steps, hospitals and healthcare institutions can have confidence that they’re working with qualified and competent physicians who meet the highest standards of patient care. However, it’s worth noting that this process can be time-consuming and expensive. It’s why many organizations turn to software and services like MedTrainer to help streamline and optimize the credentialing process.
The Costs of Not Credentialing
If you’ve ever found yourself buried in files and multiple Excel spreadsheets while working on physician credentialing, you might’ve wondered whether it’s worth all the effort. However, once you learn that failing to thoroughly credential physicians can have serious consequences that far outweigh the time and cost involved in the process, it’s easier to see its necessity.
Risk of Fines and Legal Penalties
Under “incident to” rules, there are different standards for billing across payers and states, and even a small error can lead to costly fines and additional work.
Inexperienced Physician Errors
New doctor mistakes cost the facility both in terms of damages and reputation. Proper credentialing protects every party interacting with the physician.
Risk of Hiring Excluded Physicians
The Office of Inspector General for the Department of Health and Human Services maintains a list of individuals and entities excluded from federally funded healthcare programs, including those convicted of Medicare or Medicaid fraud.
The question is not whether to credential, but rather how to do it effectively. It ensures that hospitals work with qualified and competent physicians who meet the highest standards of patient care, reducing the risk of legal penalties and reputation damage.
The Cost of Credentialing Delays
In the process of credentialing providers, time is of the essence. Every day without proper credentialing means losing revenue for the provider and the organization. Moreover, the longer it takes to complete the process, the higher the risk of losing high-caliber providers.
The manual credentialing process takes around 180 days. Here’s how it breaks down:
- 30-60 days for location onboarding and provider document acquisition
- 90-180 days for initial primary source verification and initial OIG exclusion checks
- ~4-8 hours uninterrupted per provider/payer to complete payer enrollment, facility privileging, provider profile management, CAQH profile management, payer calls, and payer market research
While manual credentialing may seem like a necessary evil, it’s far more time-consuming and prone to errors than automated systems. Using a credentialing service like MedTrainer can help organizations reduce their credentialing expenses by an average of 50%! More importantly, MedTrainer customers can credential providers three weeks faster, on average.
Get secrets to speed up your credentialing process.
The Costs of Various Physician Credentialing Methods
Credentialing is a vital task for healthcare organizations, and the costs associated with it can vary depending on several factors, including:
- Current credentialing status
- Number of physicians
- The growth rate of the practice
- Number of payers to be enrolled with
- Changes in insurance contracts or providers
- Other services provided by the credentialing provider
On average, the cost of physician credentialing is approximately $2,000-$3,000 per year. Here’s a breakdown of the costs associated with individual pieces of the credentialing process:
- Individual physician credentialing costs between $100-$200 per physician. Most insurances and facilities require recredentialing every two years, which may vary.
- The CAQH Proview database is an option for online provider data collection. The initial setup cost is $200-$500, and basic database management can cost around $50-$100 per month, depending on the level of involvement from the credentialing provider.
- Insurance panel applications usually cost around $100-$200.
These costs add up fast; however, they’re nothing compared to the costs that can accompany the fines and fees following the mistakes of an uncredentialed physician.
In-House Credentialing
Medical credentialing is a necessary process you can do in-house using a team of professionals.
According to Salary.com, the average medical staff credentialing specialist salary in the United States in 2023 is $43,558. Depending on the number of providers, locations, and payers, you may need to hire multiple specialists and support staff. Remember to also factor in office space, equipment, benefits, training, retention, and replacement costs. Often, an organization’s credentialer also has many other responsibilities, such as scheduling, billing, negotiating contracts, human resources, and more. Given the time-consuming and demanding nature of the credentialing process, an efficient process may come at the expense of other essential tasks in a busy healthcare environment.
Credentialing Software
Cloud-based credentialing software offers the ability to manage unlimited candidate data online, in one platform, making it much easier to access and track. The best credentialing software also offers automations (such as exclusion checks and license verifications) to keep your workflows on track. These time-saving automations, combined with automatic reminders and all credentialing data in one place, can reduce credentialing timelines by up to 50%.
While you will pay for the software, your credentialers will be able to get more accomplished in less time, so you may actually save money if your providers are credentialed and enrolled with payers more quickly.
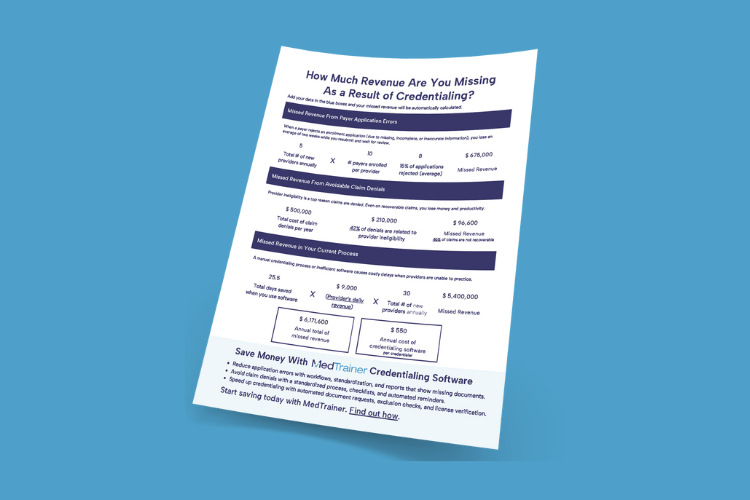
Find out how much revenue your provider credentialing process is losing.
Outside Credentialing Service
Outsourcing credentialing services means that a third-party service takes care of all (or most) credentialing tasks, including primary source verification, payer enrollments, facility privileging, and recredentialing, among other things. This option may seem like the highest cost at first, but be sure to consider all employment costs of having someone in-house, and consider the speed with which a team of outside credentialing specialists can work.
There are many benefits to outsourcing credentialing services, including:
Time-Saving
The credentialing process can be incredibly time-consuming. Outsourcing it to a third-party service frees up time and resources for healthcare organizations to focus on core business functions.
Reduced Errors
Third-party credentialing services have dedicated staff and technology that can help reduce the risk of errors and improve the accuracy of the credentialing process.
Cost-Effective
Outsourcing credentialing services can be cost-effective in both time and money. Third-party services can reduce the time and money spent on credentialing.
Compliance
Outsourcing credentialing services can help ensure healthcare organizations comply with state and federal regulations.
Access to Expertise
Third-party credentialing services often have experts knowledgeable about the latest standards and best practices.
Choosing the Right Option for Your Healthcare Organization
There’s no “best” method of credentialing providers, although, it’s not advisable to try managing the process using paper and spreadsheets. It comes down to what will work best for your organization. If you are hiring providers faster than you can credential, it may be worth paying a premium to get those healthcare professionals in front of patients faster. But, if you’ve got a great team in-house and they need a little help, enterprise credentialing software could be your best bet.
MedTrainer can help, no matter what you decide. See for yourself.
